Dimension 2
Expand Comprehensive Offerings
Like the branches that extend outward in multiple directions, the services dimension expands the array of offerings and access points across the care continuum, reaching into communities to meet diverse needs wherever people are.
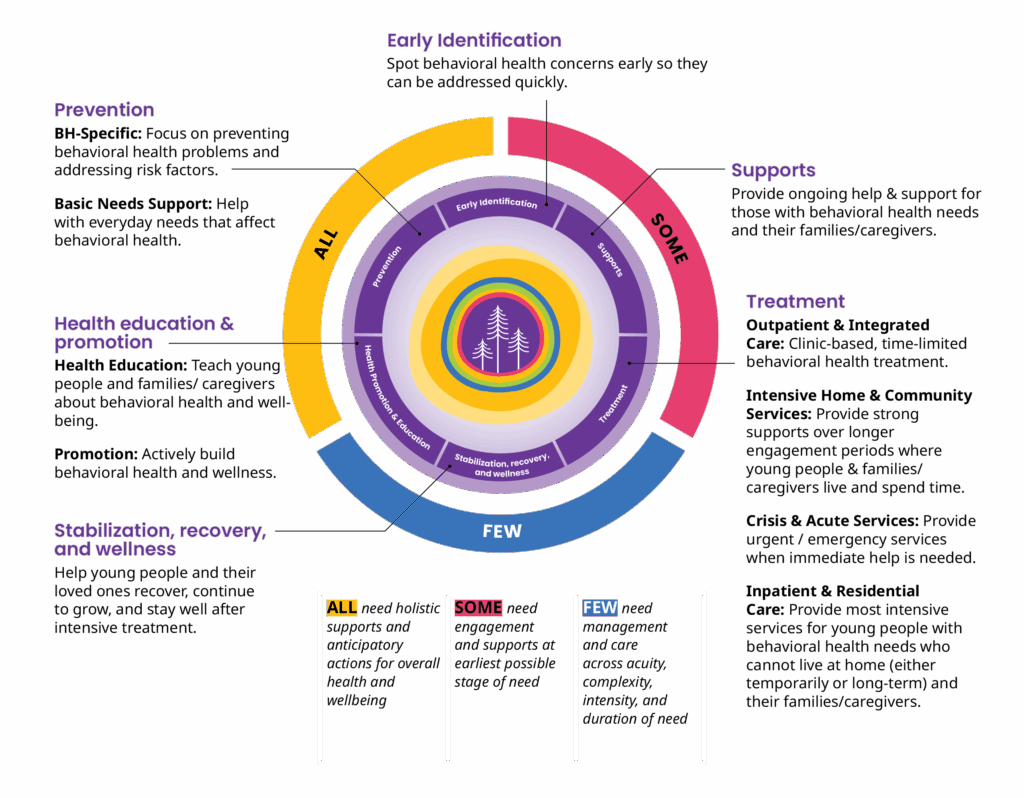
Each young person and family is unique and needs different support at different times. Washington must have diverse offerings that create flexible and adaptive support to ensure comprehensive care.
Caregiver story
The Impact of a Fragmented System on Caregivers and Families
“There needs to be a holistic look at each person that stops separating mental health from physical health.”
Caregiver story
When behavioral health and medical teams work in isolation, critical symptoms—whether behavioral or physical—can be overlooked, preventing clinicians from seeing the whole person. This fragmentation allows treatable conditions to worsen and can lead to missed or delayed treatment needs. One parent shared how her child’s care journey highlighted the importance of looking at the whole picture. While her child received support for behavioral health challenges, it took time to identify the underlying medical factors that were contributing to their symptoms. This experience reinforced for her the value of integrated care. Read more here.
Support Through Developmental Stages
Behavioral health needs emerge and change predictably as young people grow, creating both risks and opportunities that require services and supports to fit each developmental stage for young people and their families.
Perinatal Period
Comprehensive perinatal wellness supports for the parent–infant pair and family unit; normalize mental health, eliminate screening bias, and create family-based treatment pathways using harm reduction and family preservation approaches.
Support in Relevant Settings
Embed support where young people and families already are to reduce stigma and increase access.

- At home: Mobile and in-home supports, home visiting, crisis stabilization, and respite that meet families in real contexts.
- In primary care: Embedded behavioral health in pediatrics and family medicine, routine screening, bi-directional referral, and coverage.
- In educational settings: Insurance-blind multi-tiered systems of support; universal, targeted, and intensive supports in inclusive environments.
- In community “third places”: Libraries, family resource centers, faith orgs, clubs, and youth spaces that foster connection, reduce isolation, and surface needs early.
- Mobile and virtual: Rapid mobile crisis teams and tele-supports reaching rural, unhoused, and hard-to-access locations.
About Us
Support for Access and Coordination
In order to be most effective, services must operate independently of conflicts of interest or create the ability to self-refer.
- Information and navigation: Coordinated infrastructure connects young people and families with trusted providers who guide them to all available resources regardless of agency.
- Advocacy and support for caregivers: Dedicated advocates help caregivers and families navigate complex systems and manage behavioral health challenges without conflicts of interest.
- Sequencing and connecting care: Services are sequenced appropriately, complement each other, and adapt to changing needs over time with flexible funding required for providing complex care.
- Supported transitions: Warm handoffs, securely shared information, and planned transitions at life milestones prevent young people from falling through gaps.
- Team based and multidisciplinary care: Providers collaborate and consult across the system so each works at the top of their scope, improving safety, quality, and provider well being.
Support for Young People With the Most Significant and Complex Needs
Washington needs to strengthen its care capacity for young people with co occurring needs, serious mental illness, those involved in multiple systems, and those with specialized needs requiring intensive care.
- Intellectual and/or developmental disorder and autism spectrum disorder (IDD/ASD): Integrated services address behavioral health with IDD/ASD using adapted communication, daily living supports, and team based care at all intensities.
- Co occurring substance use disorder and mental health needs: Dual capable programs treat mental health and substance use together with trained staff, suitable assessments, and flexible, integrated plans.
- Serious mental illness: Community foundations plus access to intensive inpatient or residential care as needed, with medication management and relapse prevention.
- Multiple system involvement: Specialized, trauma informed services coordinate across justice, child welfare, disability, homelessness, veteran, and education systems.
- Other specialized care: Eligibility and design orient to whole person need, for example eating disorders, Fetal Alcohol Spectrum Disorder, and non substance use addictive disorders, rather than rigid labels.